Translate this page into:
Video Occulography-Assisted Diagnosis of BPPV and Comparison of Pre- and Post-Intervention Dizziness Handicap Inventory Score
Address for correspondence Richa Agrawal, MS ENT, DNB (ENT), Department of ENT, Choithram Hospital and Research Centre, Indore-452014, Madhya Pradesh, India (e-mail: agrawal23richa@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Benign paroxysmal positional vertigo (BPPV) is a commonly recognized vestibular disorder which is characterized by brief periods of vertigo and a characteristic nystagmus. The nystagmus is often difficult to appreciate with naked eyes and hence video oculography is a helpful tool. Dizziness Handicap Inventory is an objective way to assess the impact of vertigo on quality of life.
Objective
Our study here aims at diagnosing undiagnosed, difficult and missed cases of BPPV using video-oculography and managing it with repositioning manoeuvre. This study also aims at measuring Dizziness Handicap Inventory Scores pre and post repositioning manoeuvre. We also observed the association between Vitamin D levels and the occurrence of BPPV.
Methods and Materials
One hundred and twenty-six patients were enrolled in the age group of 18-70 years. After recognizing patients with BPPV, vertigo evaluation was performed. Those patients with suggestive history and suspicion of multiple canal involvement were taken for video-oculography.
Results
Forty-four patients were in age group of 50-60 years, having female predominance. 35.71% cases which were missed on clinical examination were correctly diagnosed using video-oculography. The mean pre-intervention DHI was 41.29 ± 15.90 which lowered down to 14.84 ± 11.52 in post-intervention period. The highest DHI scores were seen in multi-canal BPPV involving lateral and posterior semi-circular canals.
Conclusion
With the help of vide-oculography we could diagnose more cases of anterior and multi canal BPPV which are often missed. Maximum number of participants had insufficient levels of Vitamin-D and in our opinion correcting it would reduce the occurrence and recurrence rate.
Keywords
balance diseases
BPPV
Dizziness Handicap Inventory
video-oculography
Introduction
Vertigo and dizziness cover several multisensory and sensorimotor syndromes of various etiologies and pathogenesis. It may be central or peripheral in origin.1 Benign paroxysmal positional vertigo (BPPV) is a commonly recognized vestibular disorder, accounting for approximately one-third of the cases. It is characterized by brief periods of vertigo triggered by a changing head position relative to gravity.2 The first clinical description of positional vertigo is attributed to Barany in 1921 and in 1952, Dix and Hallpike were the first to clearly describe the provoking maneuvers.3
BPPV have an estimated lifetime prevalence of 2.4%. In studies of both young adults and the elderly, a prevalence of 9% has been described.3 The incidence of BPPV increases with age. BPPV is often unrecognized in older adults. Epidemiologically, fourth and fifth decades of life are the most commonly afflicted age groups but may also affect the younger population. There has been reported to be higher incidence in females.4
BPPV affects the calcium carbonate crystals, otoconia, in the sensory organs of inner ear, macula of utricle and saccule. They have a greater density than the surrounding endolymph, thus making the macula sensitive to changes in linear acceleration and, importantly, gravity. The semi-circular canals, in contrast, are sensitive to changes in angular acceleration. In BPPV, otoconia from the utricle is thought to collect in the semi-circular canals, making them abnormally gravity sensitive. The net result is that changes in the head position with respect to gravity result in an abnormal displacement of the cupula and stimulation of the corresponding vestibular afferents. This results in the characteristically abnormal eye movements and vertigo.3
Most cases of BPPV are idiopathic in origin and probably result from the degeneration of the macula. Some risk factors can increase its incidence such as old age, osteoporosis, vitamin D deficiency, and vertebro-basilar insufficiency.5 Several studies indicated the association between BPPV with osteoporosis and vitamin D deficiency, implying that abnormal calcium metabolism may underlie BPPV.6 Secondary causes of BPPV refer to identifiable causes of otoconial dislodge- ment. These include otologic and non-otologic surgery, head trauma, vestibular neuritis, and Meniere's disease and sudden sensorineural hearing loss.7
Any of the semi-circular canals can be affected by BPPV, but in the great majority of cases, only the posterior canal (8090%) is involved although occasionally the lateral (5-10%) and the anterior semi-circular canal (1-2%) is affected. Unilateral BPPV is much more common than bilateral involvement. BPPV that simultaneously involves multiple canals is rare and usually affects canals in the same labyrinth. The elicitation of more than one pattern of nystagmus by the positional and positioning maneuvers suggests a combined lesion that affects more than one semi-circular canal at the same time.8
The definite diagnosis of BPPV requires diagnostic positional maneuvers that lead to the observation of a canal specific positional nystagmus. Positional testing involves the provocation of vertigo and nystagmus, and different maneuvers test different semi-circular canals, e.g., DixHall Pike maneuver for posterior semi-circular canal, supine head roll test for lateral semi-circular canal, supine head extension maneuver for anterior semi-circular canal. A canal specific response is diagnosed when a rotation of the head in the plane of a semicircular canal evokes positional nystagmus of maximal intensity (in terms of slow phase velocity).
Frenzel goggles or video-oculography can be helpful, particularly when the nystagmus is weak or momentary9 The VNG examination provides a unique opportunity for the simultaneous quantitative and qualitative assessment of both horizontal and vertical components of nystagmus.10 It also assesses the function of the vestibular end organs, central vestibulo-ocular pathway, and oculomotor processes.11 The nystagmus in BPPV has a crescendo-decrescendo characteristic, and the fine ocular responses, most of the time, are difficult to be seen through Frenzel glasses. Using video-oculography, we can also record the characteristic of nystagmus. The ocular responses on record can be repeatedly examined and analyzed, which ensures reliable evaluation.12
An objective way to assess the impact of vertigo on the quality of life. The 25-item Dizziness Handicap Inventory (DHI) was developed by Gary Jacobson and Craig Newman to evaluate the self-perceived handicapping effects imposed by vestibular system disease. The items were sub-grouped into three content domains representing functional, emotional, and physical aspects of dizziness and unsteadiness.13 Total scores range from 0 to 100 with increasing scores signifying greater perception of handicap because of dizziness. The scoring for the dizziness handicap is done as follows: 16 to 34 points (mild handicap), 36 to 52 points (moderate handicap), 54+ points (severe handicap)14 (►Fig. 1).
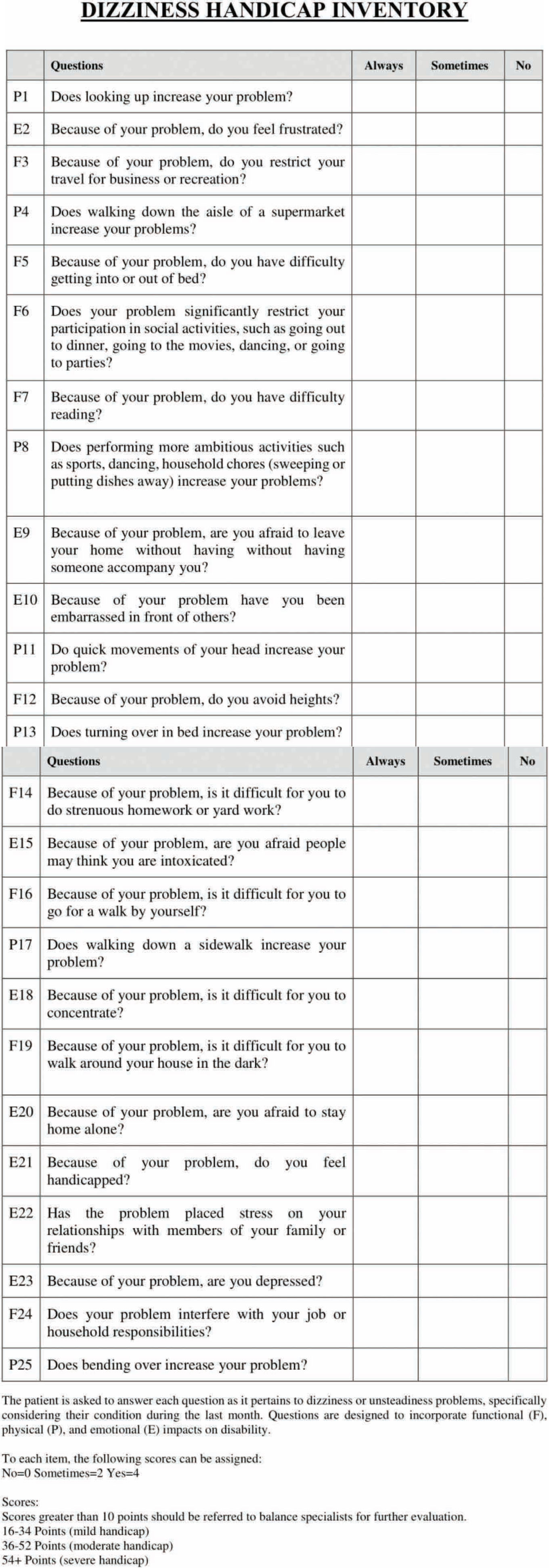
- Dizziness Handicap Inventory Score
Our study here aims at diagnosing more and more patients with complaints of vertigo associated with head and neck movements suggestive of BPPV and managing it with repositioning maneuver. This study also aims at measuring the Dizziness Handicap Inventory pre and post repositioning maneuver and reducing handicap with directed management.
Methods and Materials
The patients presented to OPD or admitted in the Department of Otorhinolaryngology and Head & Neck Surgery, Choithram Hospital & Research Center (CH &RC), Indore, Madhya Pradesh, were included in the study after obtaining a written informed consent. History was documented and clinical evaluation was performed to differentiate peripheral from central causes of vertigo. Positional tests were undertaken to provoke BPPV. In those subjects with a strong history suggestive of BPPV and the absence of nystagmus on clinical positioning tests were further studied with video-oculography. Similarly, those patients showing a classical single canal involvement but with atypical accessory nystagmus (suspected of multi-canal involvement) were further evaluated with video-oculography. With video Frenzel glasses, we documented the characteristic of nystagmus to isolate the semi-circular canal/s that were involved in the causation of vertigo. Serum Vitamin D levels were checked. The repositioning maneuver were performed subsequently for respective canals. The Dizziness Handicap Inventory was documented pre and post repositioning maneuvers.
As per the statistical calculations, 126 samples were included in the study.
Results
Majority of the patients were in the age group 51 to 60 (44 patients) years and 61 to 70 years (37 patients) and mean age of 53.07 ± 12.24 with female predilection (69 females and 57 males). In 81 (64.3%) patients, the posterior canal was involved and Epley's maneuver was performed for them; in 39 (30.9%) patients, the lateral canal was involved, Barbecue roll maneuver was performed; in 26 (20.6%) patients, the anterior canal was involved for which Yacovino maneuver was performed (►Fig. 2). Multi canal involvement was seen in 20 patients. Canal with more intense nystagmus was reposited first.

- Distribution of BPPV according to canal involvement
In 106 (84.1%) patients, only one canal was involved, while in 20 patients (15.8%), multiple canals were involved. Left side was more common in lateral canal BPPV, whereas the right side was found more common in posterior canal BPPV.
The mean pre-intervention Dizziness Handicap Inventory Score was 41.29 ± 15.90 and the mean post-intervention Dizziness Handicap Inventory score was 14.84 ± 11.52. The difference was found to be statistically significant (p = 0.001), showing a significantly lower post-intervention score (►Figs. 3 and 4). In the post-intervention period, at the end of 14 days, 84 (66.7%) patients were totally asymptomatic, 31 patients (24.6%) had mild DHI score, while 11 patients (8.7%) had moderate DHI score. In total, 95 patients (75.4%) required single repositioning maneuver, 23 patients (18.3%) required two maneuvers, while 8 (6.3%) patients required three maneuvers for relief. Theses maneuvers were repeated at an interval of 3 days.

- Comparison of pre- and post-intervention DHI severity score

- Comparison of mean pre- and post-intervention DHI score
Forty-five patients were taken for video-oculography. Twenty-five patients, who were undiagnosed on clinical evaluation could be correctly diagnosed with video-oculography. Rest 20 cases, the patients who showed a classical single canal involvement but with atypical accessory nystagmus (suspected of multi-canal involvement) on clinical positional testing were diagnosed as multi-canal involvement on VOG.
In our study, 117 patients had vitamin D levels below the normal range, 56 (44.4%) patients had deficient levels (< 25 nmol/L), while 61 (48.4%) patients had insufficient levels of vitamin D (25-75 nmol/L). Only nine (7.1%) patients had sufficient levels (> 75 nmol/L) (►Fig. 5). None of the patients had vitamin D levels in the potentially toxic range. The association between the vitamin D status and the number of maneuvers required was found to be statistically not significant.

- Distribution as per vitamin D levels
Discussion
BPPV is a subset of vertigo that is triggered with the stimulation of the vestibular system. Most commonly, it is a disease of elderly women. The dizziness due to BPPV causes moderate handicap in most cases and can be very easily treated with repositioning maneuvers.
The diagnosis and the treatment of BPPV have been assisted with the invent of video-oculography. The video Frenzel goggles help to pick up the weak nystagmus, which is not appreciated by the naked eyes. The video Frenzel goggles allow us to record eye movements and nystagmus both with and without fixation.
The studies by von Breveren et al, Furman et al, Swain et al, Shim et al found mean ages of 49.4 (SD 13.8),4 54 years,15 41.4 years,2 and 54.4 ± 14.816 respectively. These findings were consistent with our findings of mean age of 53.07 ± 12.24 years. All these studies had shown female preponderance similar to our study.
Korres et al17 and Balatsouras et al18 had shown involvement of anterior canal BPPV in 1 to 2% cases, while Jackson et al19 and Lopez-Escamez et al20 reported anterior canal BPPV in 21.2% cases and 17.14% respectively. The later findings were consistent with findings of our study (20.6%).
Shim et al,16 Tomaz et al,8 Balatsouras’18 and Lopez-Escamez et al20 had reported multi-canal involvement in 4.6%, 1.5%, 9.3%, and 20% of cases, respectively. In our study, multiple canals were involved in 20 out of 126 cases. Jackson et al,19 Lopez-Escamez et al,20,21 and Maslovara et al22 had shown importance of video-oculography in their studies for precise and accurate diagnosis of anterior canal BPPV and multiple canal involvement. The use of video-oculography has proven beneficial in our study too, where 45 cases out of 126 were diagnosed correctly.
Whitney et al and Martens et al,23,24 van der Zaag-Loonen et al,25 Nishino et al,26 and Amrish et al,27 have reported higher Dizziness Handicap Inventory score in cases of BPPV. This was similar to the findings of our study with mean pre-intervention score of 41.29 ± 15.90 and the mean post-intervention score of 14.84 ± 11.52. Eighty-four patients were asymptomatic, 31 patients had mild DHI score, while 11 patients had moderate DHI score after repositioning maneuver (►Figs. 3 and 4). The maximum pre-intervention DHI was found in cases of anterior canal involvement, which was 44.31 ± 15.37.
Buki et al,28 Jeong et al,29,30 and Sheikhzade et al31 had shown correlation between vitamin D deficiency and BPPV. These studies had also reported to be higher recurrence rate of BPPV in vitamin D deficiency. In our study also, 117 patients had vitamin D levels below the normal range. Fifty-six (44.4%) patients had deficient levels (< 25 nmol/L), while 61 (48.4%) patients had insufficient levels of vitamin D (25-75nmol/L) (►Fig. 5).
Conclusion
Video-oculography is a helpful tool in the diagnosis and treatment of benign paroxysmal positional vertigo. It not only helps us to detect the weakest of nystagmus but also correctly diagnose the involvement of canals. Dizziness Handicap Inventory is an objective way to assess functional performance in patients having vestibular disease. The higher number of asymptomatic patients in the post-intervention period in our study lead us to conclude that repositioning maneuvers form the main stay treatment for BPPV. Correction of vitamin D levels may help to reduce the occurrence of BPPV.
Conflict of Interest
None declared.
References
- Peripheral vestibular forms of vertigo. In: Vertigo and Dizziness: Common Complaints. Springer; 2005. p. :41-48.
- [Google Scholar]
- Prevalence of benign paroxysmal positional vertigo: our experiences at a tertiary care hospital of India. Egyptian Journal of Ear Nose Throat and Allied Sciences. 2018;19(3):87-92.
- [CrossRef] [Google Scholar]
- Benign paroxysmal peripheral vertigo. In: Watkinson JC, Clarke RW, eds. Scott-Brown's Otorhinolaryngology and Head and Neck Surgery: 3 volume set. CRC Press; 2018. p. :831-841.
- [CrossRef] [Google Scholar]
- Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710-715.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo involving multiple canals. Glob J Otolaryngol. 2017;10(5):116-117.
- [CrossRef] [Google Scholar]
- Serum levels of25-hydroxy vitamin D correlate with idiopathic benign paroxysmal positional vertigo. Biosci Rep. 2019;39(4):BSR20190142.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo. Laryngoscope Investig Otolaryngol. 2018;4(1):116-123.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo: concomitant involvement of different semicircular canals. Ann Otol Rhinol Laryngol. 2009;118(2):113-117.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo: Diagnostic criteria. J Vestib Res. 2015;25(3-4):105-117.
- [CrossRef] [PubMed] [Google Scholar]
- The use of videonystagmography head impulse test (VHIT) in the diagnostics of semicircular canal injuries in patients with vertigo. Int J Occup Med Environ Health. 2014;27(4):583-590.
- [CrossRef] [PubMed] [Google Scholar]
- Role of videonystagmography (VNG) in Epley's maneuver. International Journal of Otolaryngology and Head & Neck Surgery. 2014;3:311-317.
- [CrossRef] [Google Scholar]
- Benign paroxysmal positioning vertigo: diagnosis and therapy using video-oculographic control. ORL J Otorhinolaryngol Relat Spec. 2003;65(5):290-294.
- [CrossRef] [PubMed] [Google Scholar]
- The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg. 1990;116(4):424-427.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement characteristics and clinical utility of the Dizziness Handicap Inventory among individuals with vestibular disorders. Archives of Physical Medicine and Rehabilitation. 2013;94(11):2313-2314.
- [CrossRef] [Google Scholar]
- Benign paroxysmal positional vertigo. N Engl J Med. 1999;341(21):1590-1596.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo with simultaneous involvement of multiple semicircular canals. Korean J Audiol. 2014;18(3):126-130.
- [Google Scholar]
- Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23(6):926-932.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of single-or multiple-canal benign paroxysmal positional vertigo according to the type of nystagmus. Int J Otolaryngol. 2011;2011:483965.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior canal benign paroxysmal positional vertigo: an underappreciated entity. Otol Neurotol. 2007;28(2):218-222.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple positional nystagmus suggests multiple canal involvement in benign paroxysmal vertigo. Acta Otolaryngol. 2005;125(9):954-961.
- [CrossRef] [PubMed] [Google Scholar]
- Role of vestibular testing in diagnosis of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2009;141(1):7-9. author reply 10-11
- [CrossRef] [PubMed] [Google Scholar]
- Importance of accurate diagnosis in benign paroxysmal positional vertigo (BPPV) therapy. Med Glas. 2014;11(2):300-306.
- [Google Scholar]
- Usefulness of the dizziness handicap inventory in the screening for benign paroxysmal positional vertigo. Otol Neurotol. 2005;26(5):1027-1033.
- [CrossRef] [PubMed] [Google Scholar]
- Dizziness handicap and clinical characteristics of posterior and lateral canal BPPV. Eur Arch Otorhinolaryngol. 2019;276(8):2181-2189.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of unrecognized benign paroxysmal positional vertigo in older patients. Eur Arch Otorhinolaryngol. 2015;272(6):1521-1524.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life questionnaire application in patients before and after vestibular rehabilitation. International archives of otorhinolaryngology. 2008;12(4):517-522.
- [Google Scholar]
- Performance of DHI score as a predictor of benign paroxysmal positional vertigo in geriatric patients with dizziness/vertigo: a cross-sectional study. PLoS One. 2013;8(3):e58106.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D deficiency and benign paroxysmal positioning vertigo. Med Hypotheses. 2013;80(2):201-204.
- [CrossRef] [PubMed] [Google Scholar]
- Decreased serum vitamin D in idiopathic benign paroxysmal positional vertigo. J Neurol. 2013;260(3):832-838.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of benign paroxysmal positional vertigo with vitamin D supplementation: a randomized trial. Neurology. 2020;95(9):e1117-e1125.
- [CrossRef] [Google Scholar]
- The effect of serum vitamin D normalization in preventing recurrences of benign paroxysmal positional vertigo: a case-control study. Caspian J Intern Med. 2016;7(3):173-177.
- [Google Scholar]