Translate this page into:
Light Cupula Following Cochlear Implantation Surgery
*Corresponding author: Saúl Astray-Gómez, Department of Otorhinolaryngology, Hospital Universitari i Politecnic La Fe, Valencia, Spain. saulastray@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Astray-Gómez S, Bancalari-Díaz C, Saro-Buendía M, Castilla-Jiménez AB, Pérez-Guillén V. Light Cupula Following Cochlear Implantation Surgery. Ann Otol Neurotol. 2025;6:e012. doi: 10.25259/AONO_7_2025
Abstract
Vertigo and dizziness are common symptoms after cochlear implantation, though the mechanisms involved are numerous and complex. We present the case of a woman who developed persistent direction-changing ageotropic nystagmus in the immediate postoperative period following cochlear implant surgery. This may be explained by a light cupula mechanism triggered by the entry of inflammatory mediators into the endolymph through the cochleostomy, providing supporting evidence for some of the proposed theories underlying this phenomenon.
Keywords
Cochlear implant
Direction-changing nystagmus
Light cupula
Positional vertigo
INTRODUCTION
Cochlear implant surgery is a well-established treatment modality for severe-to-profound sensorineural hearing loss, with remarkable success in restoring auditory function. Like any other surgical procedure, it is not exempt from complications. Most are mild and temporary, including facial palsy, dysgeusia, tinnitus, local infection, or skin disorders. Vertigo and dizziness are among the most common, although the underlying mechanisms are highly diverse. A high index of clinical suspicion and a thorough physical examination are key to achieving an accurate diagnosis.
CASE REPORT
We present the case of a 54-year-old woman with bilateral sensorineural hearing loss due to the administration of ototoxic drugs during an intensive care unit admission 20 years ago. She reported progressive worsening of symptoms in recent years, particularly in the right ear, along with poor performance of bilateral auditory prostheses. Audiological assessment confirmed profound bilateral sensorineural hearing loss. Preoperative imaging studies, including mastoid CT and MRI, revealed no anatomical abnormalities or malformations in the middle or inner ear. She was scheduled for right-sided cochlear implantation, which was performed uneventfully.
Two days postoperatively, she was discharged without complications, except for mild dizziness and a tension-type headache. Otoneurological examination was unremarkable at that time. However, five hours later, she was readmitted to the Emergency Department with sudden-onset severe vertigo, nausea, vomiting, and postural instability, which began while she was lying in bed.
Otoneurological evaluation revealed horizontal geotropic direction-changing nystagmus on the McClure diagnostic manoeuver, without latency, fatigability, or exhaustibility. The head impulse test showed no saccades, and the cover test was negative. No other neurological deficits were noted. Based on these findings, she was hospitalised for symptomatic management and further evaluation.
Video head impulse testing demonstrated normal vestibulo-ocular reflex gain bilaterally. Videonystagmography (VNG) revealed no spontaneous nystagmus in the seated position. Positional testing reproduced the initial findings. A null point (the head position in which the nystagmus is suppressed) was observed when the head was tilted 25–30° towards the right side [Figure 1]. These findings were consistent with the diagnosis of a light cupula affecting the right lateral semicircular canal.
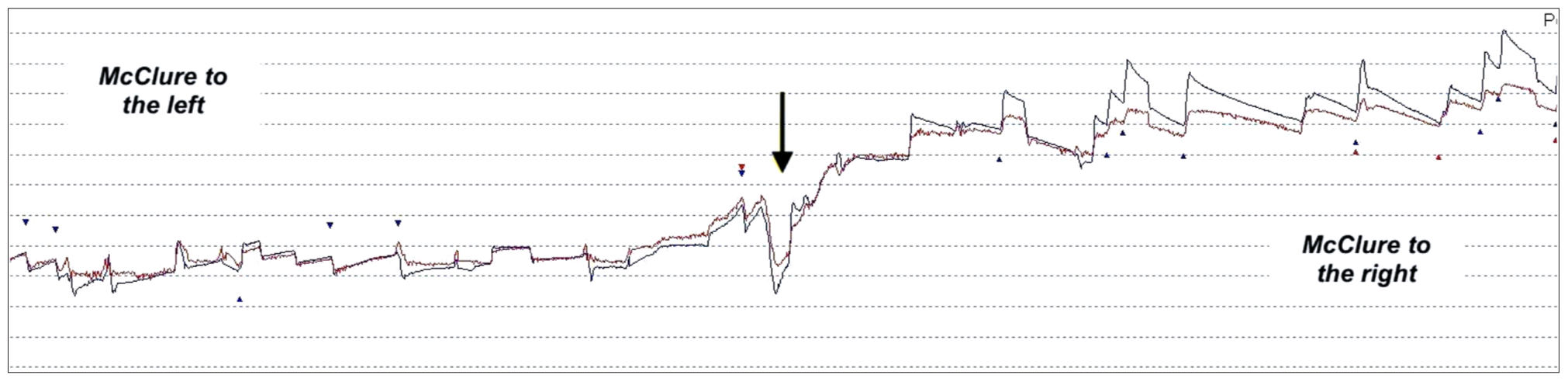
- Videonystagmography recording showing geotropic direction-changing nystagmus during the McClure maneuver. The null point (black arrow) indicates the head position at which the lateral semicircular canal’s cupula aligns with gravity and nystagmus is suppressed. The red line corresponds to the movement of the right eye, and the blue line to the left eye. The red and blue arrows indicate the points where the fast phases of the nystagmus (saccades) occur.
She received intravenous amoxicillin/clavulanate, methylprednisolone, diazepam, and nonsteroidal anti-inflammatory drugs for symptomatic relief. Nystagmus characteristics were monitored daily. On day six, she was discharged following the complete resolution of symptoms and the disappearance of nystagmus.
DISCUSSION
Vestibular symptoms—such as vertigo, dizziness, or balance disturbances—are among the most frequently reported postoperative complaints following cochlear implantation, with an incidence ranging from 32% to 74%, depending on the study and diagnostic criteria used.1 The impact of cochlear implantation on cochleovestibular function has been widely investigated, but results remain inconclusive. While comprehensive vestibular assessments before and after implantation are recommended, they have not proven predictive for symptom occurrence or persistence.2
Positional vertigo accounts for a small proportion of these cases (approximately 1%) and is infrequently reported in the literature, with benign paroxysmal positional vertigo (BPPV) identified as the main mechanism. A higher prevalence is noted among women (7:1), and no significant population-wide risk factors have been identified.3
Various pathophysiological mechanisms have been proposed, including direct trauma to otolithic organs from the electrode tip, indirect trauma from drill-induced vibrations, and otolith displacement secondary to electrical stimulation spread from the implant.4 The precise impact of each remains unclear, likely varying based on patient-specific factors and surgical technique. A significantly increased risk of vertigo has been observed with cochleostomy compared to the round window approach.5
Vibratory trauma appears to play a key role, suggesting that mechanical factors leading to otoconial displacement are central to symptom development. Recently, there has been growing interest in cases of persistent direction-changing positional (PDCP) nystagmus that do not conform to classic diagnostic criteria. This has led to the proposal of the “light cupula” mechanism as an explanation for horizontal, direction-changing nystagmus observed in supine patients whose heads are tilted 25–30° upwards.6,7
The light cupula hypothesis originated from the concept of positional alcoholic nystagmus (PAN), which posited that alcohol diffuses more rapidly into the cupula than the surrounding endolymph, creating a temporary density gradient.8 The nystagmus associated with light cupula typically exhibits the following characteristics: (1) purely horizontal, (2) direction-changing with sagittal head movement, (3) absent latency and fatigability, (4) presence of a null point with head tilted 20–30° toward the affected side, and (5) absence of central neurological signs.
Since light cupula and lateral semicircular canal (LSCC) canalolithiasis present with similar clinical features, careful observation of the nystagmus is essential. VNG is particularly helpful. In LSCC canalolithiasis, nystagmus typically lasts less than one minute, has latency and fatigability, and lacks a null point. Central causes must also be considered in the differential diagnosis, such as vestibular migraine9 or structural abnormalities like medullary infarction or cerebellar tumors.10 These may be accompanied by additional signs such as impaired horizontal smooth pursuit.
Kin et al. reported a case of PDCP nystagmus after otologic surgery involving a 55-year-old woman who developed vertigo following posterior tympanotomy and ossiculoplasty with prosthesis implantation for chronic otitis media with cholesteatoma.11 Disruption of the oval window during stapes manipulation was proposed as the cause. Similarly, in our case, communication between the middle and inner ear may have triggered the process, with inflammatory mediators entering the vestibular endolymph and altering its density relative to the cupula.
Light cupula–induced vestibular syndrome may be underdiagnosed following cochlear implantation due to limited clinical awareness or inadequate physical examination. Although many episodes of postoperative vertigo are mild and nonspecific, positional manoeuvers provide valuable diagnostic information and should be systematically performed when positional vertigo is suspected. Assessment of nystagmus duration and identification of a null point are crucial for differential diagnosis. VNG remains an essential tool for detailed evaluation. Although vestibular function is generally preserved, it should still be assessed.
Light cupula does not constitute a distinct disease entity but rather represents a transient pathological condition of the inner ear. Its pathophysiology is still poorly understood, and no specific treatment protocols currently exist. Canalith repositioning manoeuvers used for BPPV are ineffective. Management focuses on symptom control, including vestibular rehabilitation, head position adjustments, and lifestyle modifications. In refractory cases, pharmacological vestibular suppressants may be considered.6
CONCLUSION
Light cupula, presenting as geotropic direction-changing persistent nystagmus, may be a postoperative complication of otologic surgery. A communication between the middle and inner ear appears to be a key precipitating factor. Thorough physical examination and judicious use of diagnostic tools are essential for accurate differential diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Vertigo Following Cochlear Implantation: A Review. Int J Res Med Sci. 2022;10:570-575.
- [Google Scholar]
- Predictive Factors for Subjective Vertigo Following Cochlear Implantation: A Regional Multicenter Cohort Study of 395 Patients. Otol Neurotol. 2024;45:e18-23.
- [CrossRef] [PubMed] [Google Scholar]
- Benign Positional Vertigo After Cochlear Implantation. Otolaryngol Head Neck Surg. 2005;132:741-5.
- [Google Scholar]
- Meta-Analysis of Subjective Complaints of Vertigo and Vestibular Tests After Cochlear Implantation. Laryngoscope. 2018;128:2110-23.
- [CrossRef] [PubMed] [Google Scholar]
- The Light Cupula: An Emerging New Concept for Positional Vertigo. J Audiol Otol. 2018;22:1-5.
- [Google Scholar]
- Persistent Geotropic Direction-Changing Positional Nystagmus with a Null Plane: The Light Cupula. Laryngoscope. 2014;124:E15-9.
- [Google Scholar]
- Role of Semicircular Canals in Positional Alcohol Nystagmus. Am J Physiol. 1965;208:1065-70.
- [Google Scholar]
- Migrainous Vertigo Presenting as Episodic Positional Vertigo. Neurology. 2004;62:469-72.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated Horizontal Positional Nystagmus from a Posterior Fossa Lesion. Ann Neurol. 2014;76:905-10.
- [Google Scholar]
- Positional Vertigo Showing Direction-Changing Positional Nystagmus after Chronic Otitis Media Surgery: Is It Benign Paroxysmal Positional Vertigo? Res Vest Sci. 2018;17:23-27.
- [Google Scholar]








