Translate this page into:
Physical Therapy for the Horizontal Semicircular Cupulolithiasis: A Prospective Interventional Case Series from an Otoneurology Center in South Rajasthan, India
Address for correspondence Ajay Kumar Vats, MBBS, MD (Medicine), DM (Neurology), FRCP, Chaudhary Hospital & Medical Research Centre Private Limited, 472-473, Sector 4, Hiran Magri, Udaipur, Rajasthan, 313002, India (e-mail: vatsneuro@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective
This article aims to study the effect of physical therapy in patients of horizontal semicircular cupulolithiasis with results audited in the short term.
Design
Nonrandomized prospective interventional study.
Study Sample
Four patients with horizontal semicircular cupulolithiasis.
Results
All four patients in whom diagnostic supine roll test (carried at least thrice to look for the sustainability as well as the polarity of the nystagmus) elicited apo- geotropic horizontal positional nystagmus lasting more than 1 minute were subjected to therapeutic head-shaking maneuver (HSM). The results were audited immediately after the physical therapy, and at 1 hour. Follow-up by telephonic interviews for 4 weeks was done in all patients. Three out of four patients responded to HSM alone. One patient who did not respond to HSM was successfully treated with four other sequent physical therapies.
Conclusion
The response of physical therapy for horizontal semicircular cupulolithiasis occasionally indicates the side of the cupula to which otoconial debris is adherent (Cup-U or Cup-C). Occasionally, Cup-C variant of horizontal semicircular cupulolithiasis can be transformed by physical therapy to long posterior arm horizontal semicircular canalolithiasis—a disorder with better established treatment options.
Keywords
balance diseases
cupulolithiasis
head-shaking maneuver
HSC-BPPV
supine roll test

[SHOW_RELATED_PUBMED_ARTICLES]
Introduction
Benign paroxysmal positional vertigo (BPPV) is a mechanical disorder of the vestibular membranous labyrinth. The main symptom is sudden vertigo provoked by changes in the position of the head relative to gravity: sitting upright from supine, lying down, and rolling over in bed, looking up, or stooping forward.1,2 Symptoms may last for days, weeks, months, or years, or could be recurrent.3 BPPV is commonly due to free-floating otoconial debris entering one or more of three semicircular canals from the utricle, which is called canalolithiasis.4,5 Uncommonly, it is due to cupuloli- thiasis, in which otoconial debris adheres to the gelatinous cupula.3,6,7 Such pathologies result in cupular deflection when the head moves to a certain position, which is secondary to the otoconial debris overcoming the hydrodynamic resistance of the endolymph in canalolithiasis and the cupula becoming heavier in cupulolithiasis.8 In either case, it results in asymmetrical stimulation of the vestibular labyrinth in situations when the head moves relative to gravity, which explains the symptom of positionally triggered vertigo.9
►Table 1 shows that 1.94 to 38% of all BPPV patients diagnosed at any specialty clinic have horizontal semicircular canal BPPV (HSC-BPPV).10-22 The supine roll test (SRT) elicits horizontal positional nystagmus (PN) in HSC-BPPV.23 Apogeotropic PN is ascribed to either cupulo- lithiasis or canalolithiasis in the ampullary short anterior arm,24-26 with cupulolithiasis being categorized as either Cup-C or Cup-U depending on the side to which otoconial mass is adherent.6,7,27 Geotropic PN is seen with nonampullary long posterior arm horizontal semicircular canalolithia- sis.28 Both will present bilaterally during SRT. The duration of the PN is up to 1 minute in the long posterior arm horizontal semicircular canalolithiasis and more than 1 minute in the cupulolithiasis. The current diagnostic criteria for horizontal semicircular cupulolithiasis (HSC-BPPV-cu) require that an apogeotropic horizontal PN elicited during SRT lasts more than a minute and remains unchanged during repetitive testing.29,30
| Authors | No. of patients | PSC-BPPV | HSC-BPPV | ASC-BPPV | Multiple canals |
|---|---|---|---|---|---|
| De la Meilleure et al,10 1996 | 287 | 78.05% | 16.38% | - | 5.57% |
| Honrubia et al,11 1999 | 292 | 85.62% | 5.14% | 1.37% | 7.87% |
| Macias et al,12 2000 | 259 | 93.02% | 1.94% | - | 5.04% |
| Korres et al,13 2002 | 122 | 90.16% | 8.2% | 1.64% | - |
| Sakaida et al,14 2003 | 50 | 56% | 38% | - | 6% |
| Imai et al,15 2005 | 108 | 64.82% | 33.33% | - | 1.85% |
| Nakayama and Epley,16 2005 | 833 | 66.39% | 10.08% | 2.28% | 21.25% |
| Cakir et al,17 2006 | 169 | 85.21% | 11.83% | 1.18% | 1.78% |
| Moon et al,18 2006 | 1,692 | 60.9% | 31.9% | 2.2% | 5.0% |
| Jackson et al,19 2007 | 260 | 66.9% | 11.9% | 21.2% | - |
| Chung et al,20 2009 | 589 | 61.8% | 35.3% | 2.9% | - |
| Vlastarakos et al,21 2019 | 96 | 90.62% | 8.33% | 1.04% | - |
| Chua et al,22 2020 | 1,542 | 92.2% | 3.7% | - | 4.08% |
Abbreviations: ASC-BPPV, anterior semicircular canal benign paroxysmal positional vertigo; HSC-BPPV, horizontal semicircular canal benign paroxysmal positional vertigo; PSC-BPPV, posterior semicircular canal benign paroxysmal positional vertigo.
Cupulolithiasis was first reported in 1969 as a granular basophilic mass attached to the cupula of the posterior semicircular canal in the temporal bone histological sections of two patients31 but a clinico-physiologic basis of its existence in the HSCs generating a long-duration, nearly nonfatigable apogeotropic horizontal PN during SRT was elaborated much later.6,7,29 In the last decade, seven prospective interventional studies32-38 have addressed patients with the apogeotropic variant of HSC-BPPV but only two34,36 out of these seven include subjects with exclusive HSC-BPPV-cu, while the others32,33,35,37,38 include those with short anterior arm canaloli- thiasis as well. Segregation of the cupulolithiasis (Cup-C or Cup-U), and its influence on the treatment of 40 patients with ostensive HSC-BPPV-cu with either one-stage (Cup-U) or two-stage (Cup-C) forced prolonged positioning (FPP) is described by the Chiou et al32 but the study possibly includes patients with short anterior arm horizontal semicircular canalolithiasis (duration of the apogeotropic horizontal PN and its unchanging character not specified).
We are reporting a case series of four patients, with HSC-BPPV-cu, who visited our center between June 2019 and July 2020. All four patients were treated with some form of physical therapy, and the results were audited in the short term immediately and after an hour. The resolution of vertigo as well as the disappearance of the apogeotropic PN, during the verifying SRT, was the endpoint of treatment with physical therapy. To the best of the authors’ knowledge, no such study of patients diagnosed with HSC-BPPV-cu has been reported from India hitherto.
Material and Methods
The study was approved by the ethics committee of the attending otoneurology center. The HSC-BPPV-cu was diagnosed as per the following criteria:
Rotational vertigo triggered by changes in the position of the head relative to gravity.
Apogeotropic horizontal PN elicited by the SRT, the side with the weaker nystagmus was considered pathological as per Ewald's second law.39
The duration apogeotropic horizontal PN elicited during the SRT lasted more than a minute and its attributes (direction and threshold duration) did not change with at least three times executed SRT.
Vertigo associated with the concomitant elicited PN.
Exclusion criteria were: BPPV treated with any form of physical therapy in the past, posttraumatic BPPV, a diagnosis of other peripheral vestibular disorders (Meniere's disease, vestibular neuritis, vestibular paroxysmia, etc.), and vertigo secondary to central nervous system disorders.
Informed consent was taken from all four participants. The general physical examination and vitals of all patients were normal. In all patients, the screening examination of the cervical spine did not reveal any limitation of movement and the examination of the back region did not reveal kyphoscoliosis. The lumbosacral spine assessment, including straight-leg raising (SLR) and reverse SLR tests, were normal in all patients. The neurological examination revealed normal cranial nerve examination; strength was grade 5/5 in all four limbs with normal deep tendon reflexes, and bilateral plantar reflexes were flexor. Examination of the cerebellar system revealed no spontaneous or gaze-evoked nystagmus, and there was no appendicular or axial incoordination. The otoneurological examination revealed normal vertical and horizontal saccadic and smooth pursuit eye movements. The head impulse test was bilaterally normal.
The pathological side is identified by the SRT. The SRT (►Videos 1, 4, and 7) is done with the patient in long-sitting on the examination table. The patient is moved to supine with her head landing on a four-inch-thick pillow, so it is anteflexed to 30 degrees in this position. The supine neutral position is maintained for 30 seconds to look for lying-down nystagmus (LDN). Thereupon, the patient's head is rotated first to one side and maintained until the elicited PN lasts. After the lateral head roll to one side, the patient's head is brought to the neutral supine position and then briskly rolled in the yaw-axis to the other side, and maintained until the elicited PN lasts. The SRT was performed multiple times (at least three times at an interval of 5 minutes) in all patients to testify the perseverance of its polarity (apogeotropic) as well as its long duration (more than a minute). Immediately after a therapeutic maneuver, and after 1 hour, a verifying SRT was repeated to assess its outcome. The patients were instructed to report next day in case the vertigo recurs. The recovery was audited in terms of the disappearance of vertigo, as well as the previously observed diagnostic apogeotropic horizontal PN. No more than five different therapeutic maneuvers were performed on any one patient in a single day. The therapeutic positional maneuvers and the physical therapies used were as under:
HSM (►Fig. 1) (►Videos 2, 5, and 8) is performed with the patient in short-sitting and lower limbs hanging along the long edge of the examination table. The head is anteflexed 30 degrees in the pitch plane and briskly shaken by the excursions of 30 degrees side-to-side in the yaw axis for around 30 seconds. Two sequent HSM are done in one session of treatment. The rapid acceleration and deceleration during HSM generate inertial forces in the otoconial debris (irrespective of the side to which it is attached) adherent to the cupula that causes its detachment or loosens it.
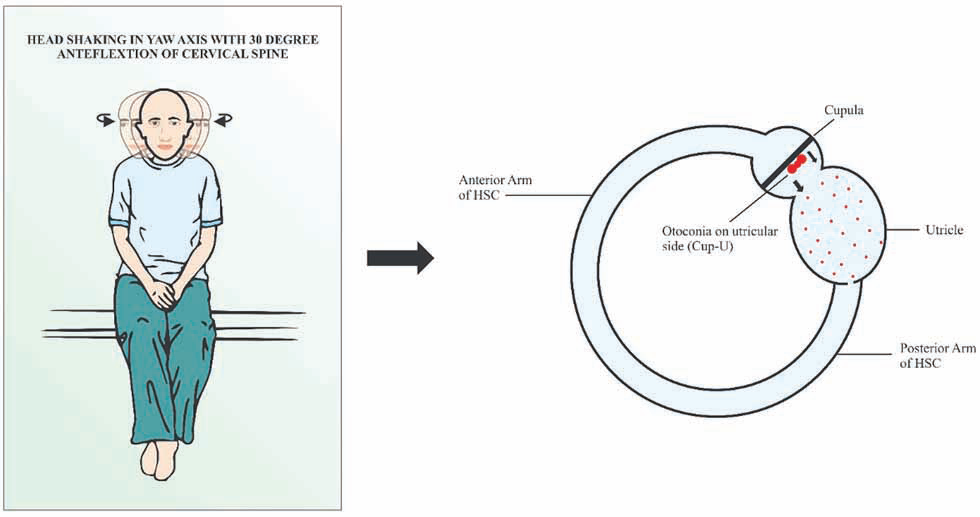
- Head-shaking maneuver (HSM). The head is anteflexed 30 degrees in the pitch plane and briskly shaken by the excursions of 30 degrees side-to-side at an approximate rate of 3 Hz in the yaw axis for approximately 30 seconds
Posterosuperior meatal oscillation with a handheld vibrator (►Video 10) is performed with the patient number 4 in the right lateral recumbent position. Oscillations are delivered to the suprameatal triangle in the posterosuperior area of the involved left ear with an electrically operated handheld vibrator (Hitachi Magic Wand with speeds: low 5,000 revolutions per minute [RPM], high 6,000 RPM) for approximately 60 seconds.
180° head-roUing maneuver40 (►Fig. 2, ►Video 12) is performed with the patient positioned supine with her head in 30 degrees flexion on a four-inch-thick pillow. The head-rolling maneuver in the supine position is executed. The head is quickly rolled towards the healthy side and slowly towards the affected ear eight times. By the generated inertial forces, quick movement is expected to detach the otoconial debris adherent to the cupula on its canal side, and the slow movement is presumed to facilitate the migration of the detached otoconial debris toward the utricle under the effect of gravitational force.
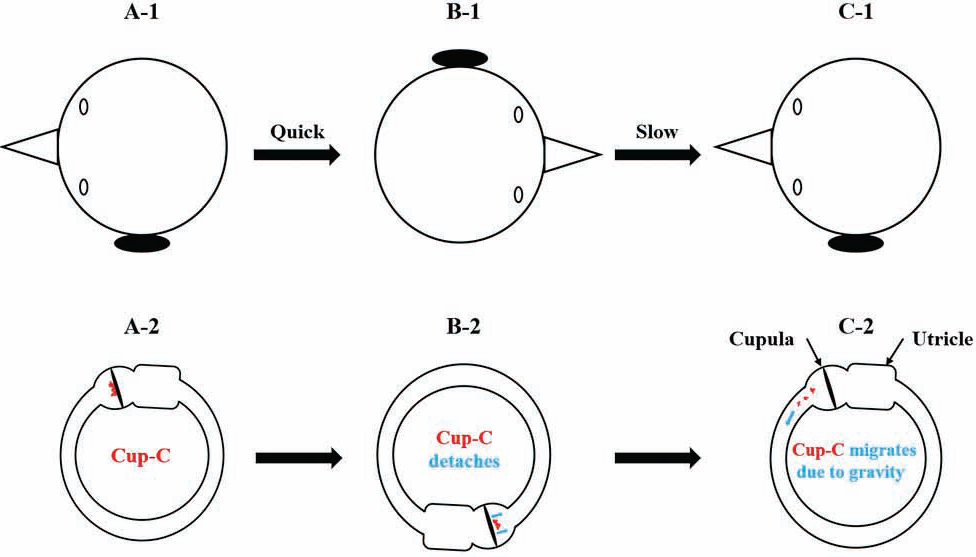
- 180-degree head-rolling maneuver in supine recumbent position. With patient in the supine recumbent position, her head is quickly rolled 180 degrees in the yaw axis from the diseased left to the healthy right side. Thereupon, it is slowly rolled back from the healthy right to the diseased left side. Plausibly the quick movement either detaches away or loosens the otoconial debris adherent to the canal side of the cupula (Cup-C) under the influence of generated inertial forces. The slow movement facilitates the migration within the horizontal semicircular canal from its short anterior ampullary arm to the long posterior nonampullary arm under the influence of gravitational force
FPP is carried by instructing the patient number 4 to position the left lateral recumbent for an hour. The rationale for left lateral recumbent FPP is to detach the otoconial debris from the canal side of the utricle under the effect of gravitational force (►Fig. 3). The otoconial debris adherent to the canal side of the cupula is plausibly loosened by the previously executed HSM and 180-degree head-rolling maneuver.
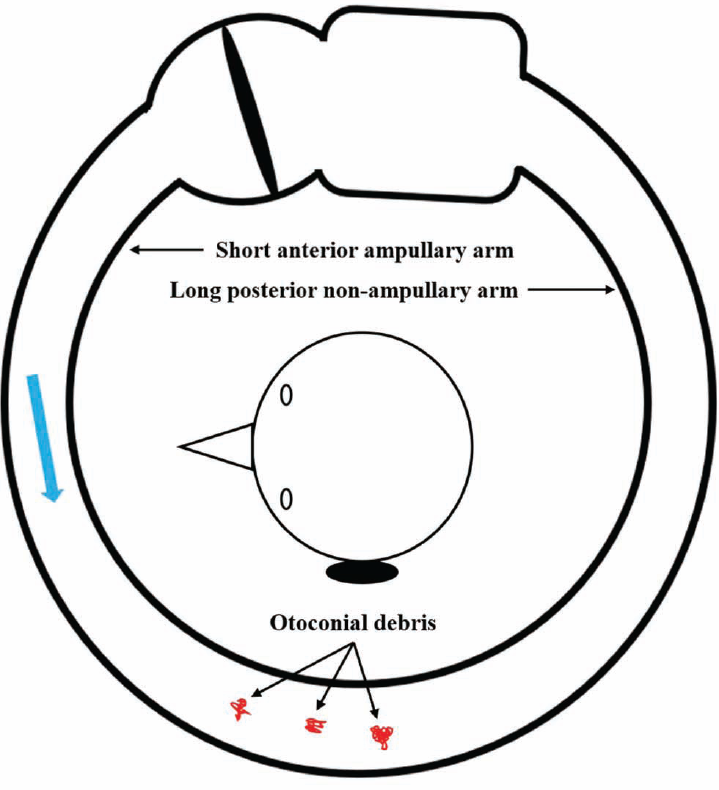
- Forced prolonged positioning (FPP) in left lateral recumbent position for 1 hour. The patient is positioned left lateral recumbent for 1 hour. In the left lateral recumbent FPP, the otoconial debris (in red), which has either detached or loosened from the canal side of the cupula, migrates (blue arrow) within the short ampullary anterior arm of the canal toward its posterior end
Gufoni maneuver (►Video 15) for the geotropic left HSC-BPPV is performed with the patient number 4 in short sitting with both lower limbs hanging down the examination table. From short sitting, she is positioned right (con- tralesional) lateral recumbent for a minute. Thereupon, her head is rotated approximately 45 degrees downwards in the yaw-axis and maintained for 2 minutes, after which she is positioned to the upright sitting.
Results
All four patients included in the study had a history of positionally triggered vertigo on lying supine, rolling to either of the side lateral positions, and on getting upright from the supine. The duration of symptoms ranged from 1 to 8 days. The initial diagnostic SRT elicited apogeotropic horizontal PN of more than a minute duration during the lateral head rolls in all four patients (►Table 2). The demographic profile, symptom duration, strength of the PN during diagnostic SRT, LDN direction, diagnosis, therapeutic physical therapy, and results of the verifying SRT are summarized in ►Table 3.
| Patient number | Diagnostic supine lateral head roll test | Click for video | |||||
|---|---|---|---|---|---|---|---|
| To right | To left | ||||||
| Latency | Duration | Relative strength | Latency | Duration | Relative strength | ||
| 1 | 4 s | 47 s | Weaker | 5 s | 173 s | Stronger | ►Video 1 |
| 2 | 4 s | 190 s | Stronger | 4 s | 60 s | Weaker | ►Video 4 |
| 3 | 3 s | 79 s | Stronger | 5 s | 74 s | Weaker | - |
| 4 | 5 s | 156 s | Stronger | 18 s | 60 s | Weaker | ►Video 7 |
Note: The latency, duration, and relative strengths of the apogeotropic horizontal positional nystagmus on lateral head roll to the right and left during the diagnostic supine roll test carried initially.
| Patient number | Age | Sex | Vertigo duration | Supine roll test (diagnostic) | Diagnosis | LDN | Physical therapy for treatment | Supine roll test (verifying) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Apogeotropic > 1 min | Immediate | At 1-h | ||||||||
| Right | Left | |||||||||
| 1. | 40 | F | 1 d | + | + + | Right apo-HSC-BPPV | Absent | HSM | No PN | No PN |
| 2. | 25 | F | 8 d | ++ | + | Left apo-HSC-BPPV | Absent | HSM | No PN | No PN |
| 3. | 51 | F | 2 d | ++ | + | Left apo-HSC-BPPV | Absent | HSM | No PN | No PN |
| 4. | 64 | F | 4 d | ++ | + | Left apo-HSC-BPPV | To left | See ►Fig. 4 | No PN | No PN |
Abbreviations: +, weaker; ++, stronger; apo-HSC-BPPV, apogeotropic horizontal semicircular canal benign paroxysmal positional vertigo; F, female; HSM, head-shaking maneuver; LDN, lying-down nystagmus; PN, positional nystagmus.
Patient Number 1,2, and 3
The patient number 1, 2, and 3 underwent therapeutic HSM (►Fig. 1) with their heads flexed approximately 30 degrees. A verifying SRT performed in all three immediately as well as at 1 hour (►Videos 3 and 6) after the HSM did not elicit apogeotropic horizontal nystagmus, and none of them had residual vertigo either. A telephonic interview was weekly taken for the next 4 weeks, and all three remained symptom free.
Patient Number 4
The long-duration horizontal apogeotropic PN (►Video 7) with perseverance on repeating the supine lateral head roll test suggests HSC-BPPV-cu. Cupulolithiasis of the left HSC is indicated by the side eliciting the weaker horizontal PN during the supine lateral head roll test as per the Ewald's second law.39 Accordingly, the patient underwent two sequent HSM (►Fig. 1, ►Video 8). A verifying SRT (►Video 9) immediately after the HSM remains unchanged. The right lateral recumbent positioning of the patient is done. Mastoid oscillations (►Video 10) are delivered to the suprameatal triangle in the posterosuperior area of the involved left ear with an electrically operated handheld vibrator for approximately 60 seconds. Immediately after the mastoid oscillation, a second verifying SRT (►Video 11) remains almost unaltered. A 180-degree head-rolling maneuver (►Fig. 2, ►Video 12) was undertaken. Plausibly the quick movement during the 180-degree head-rolling maneuver either detaches away or loosens the otoconial debris adherent to the canal side of the cupula (Cup-C) under the influence of generated inertial forces. The slow movement facilitates the migration within the HSC from its short anterior arm to the long posterior arm under the influence of gravitational force. However, a third verifying SRT (►Video 13) immediately after the 180-degree head rolling maneuver remains still unaltered. Thereupon, the patient is positioned left lateral recumbent for 1 hour (FPP) (►Fig. 3). A fourth verifying SRT (►Video 14) elicits LDN of 28 seconds duration beating to the patient's right in the neutral supine position. The lateral head rolls to the right as well as to the left elicit geotropic horizontal nystagmus of 25 seconds duration to either side. Elicited geotropic horizontal nystagmus is stronger on the lateral head roll to the left, indicating transformation to left long posterior arm horizontal semicircular canalo- lithiasis. Two sequent Gufoni maneuvers (►Video 15) are undertaken. A fifth verifying SRT (►Video 16) performed immediately, and after 1 hour neither elicited the PN nor the patient had vertigo. A telephonic interview was weekly taken for the next 4 weeks, and the patient remained symptom free. The treatment protocol of patient number 4 is summarized in ►Fig. 4.
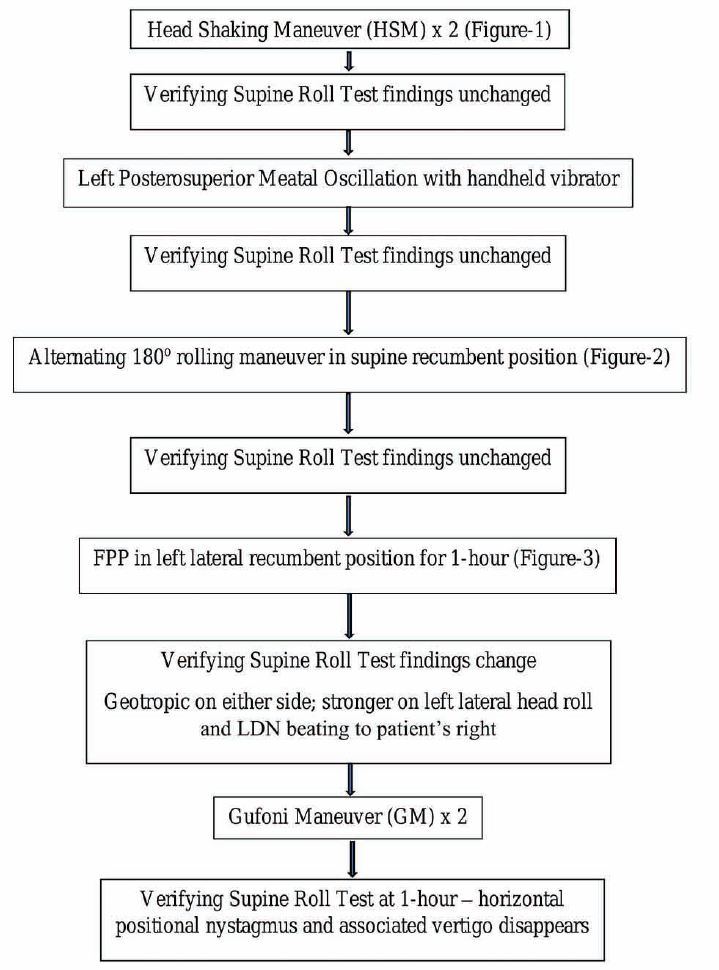
- Management algorithm of patient number 4 with Cup-C variant of left horizontal semicircular cupulolithiasis
Discussion
The apogeotropic variant of the HSC-BPPV is attributable to pathologies at three different sites within the HSC, namely (1) ampullary short anterior arm canalolithiasis, (2) Cup-U variant of cupulolithiasis, and (3) Cup-C variant of cupuloli- thiasis. A singular assessment of the apogeotropic horizontal PN by the SRT is often inadequate to decipher the precise location of the otoconial debris. The apogeotropic horizontal PN that either disappears or transforms into the geotropic variant, during SRT, is in all probability secondary to an unfixed and moveable otoconial debris within the short anterior arm of the HSC.24,41-44 By contrast, apogeotropic horizontal PN secondary to cupulolithiasis (heavy cupula) invariably lasts more than a minute and remains unaltered even after multiple sequences of the SRT.29,30 For this reason, performing multiple sequences of the diagnostic SRT is imperative to establish a diagnosis of HSC-BPPV-cu, and this was aptly executed in all four cases reported here.
Cases 1 to 3 responded immediately to HSM. Verifying SRT immediately and after 1 hour did not elicit apogeo- tropic horizontal PN, and all three remained symptom free over 4 weeks of follow-up on interviewing telephonically. HSM employs the inertia of the otoconial debris to disengage it from the gelatinous cupula. The offloading of the otoconial debris from the utricle side of the cupula would bring immediate relief in vertigo,23 and the detached debris disperses into the gelatinous matrix of the utricle (►Fig. 1). The dramatic response in patients 1 to 3 to HSM in terms of alleviation of positionally triggered vertigo as well as extirpation of the apogeotropic PN (immediately as well as after 1 hour) explicitly endorse the fact that they suffered from the Cup-U variant of HSC-BPPV-Cu.
Case 4 failed to respond to the two sequent HSM. Accordingly, we had to recourse to a series of sequent maneuvers generating the inertial forces to disengage the otoconial debris adherent to the cupula; mastoid oscillation and 180-degree head-rolling
maneuver, previously reported in the literature.34,38 Because of the failure of HSM and mastoid oscillation to abolish the apogeotropic horizontal PN and the concomitant positionally triggered vertigo, it was hypothetically inferred that otoconial debris is adherent to the canal side of the cupula. The 180-degree head-rolling maneuver (►Fig. 2) and its variants have been used previously with variable success to offload the otoconial debris purportedly adherent to the canal side of the cupula.40,43,45 The 180-degree head-rolling maneuver, and the antecedent HSM and mastoid oscillation plausibly loosened the otoconial debris adherent to the canal side of the cupula. A subsequent left lateral recumbent FPP (►Fig. 3) for 1 hour just dropped off the oto- conial debris loosely adherent to the canal side of the cupula under the effect of the gravitational force. A verifying SRT executed just after the FPP elicits an LDN to the patient's right, and geotropic horizontal PN on the lateral head roll to either side that was visibly stronger on the left side. Such a change in the polarity of the horizontal PN from apogeotropic to geotropic and reversal in the lateralization of its strength (stronger on the lateral head roll to right initially to stronger on the lateral head roll to left now) indicates transformation from Cup-C cupuloli- thiasis to long posterior arm canalolithiasis of the left HSC. The otoconial debris not only dropped off from the canal side of the cupula after the left lateral recumbent FPP but also relocated to the posterior arm of the HSC. Based on our case series, we suggest an algorithm for action when an apogeotropic horizontal PN is elicited on SRT (►Fig. 5).
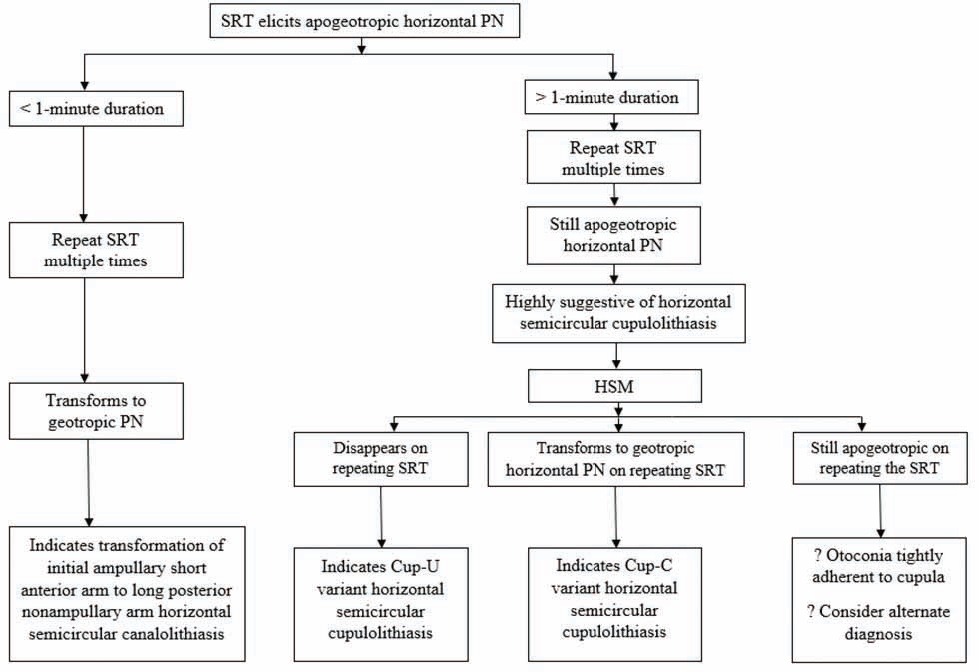
- Suggested algorithm for action when supine roll test (SRT) elicits apogeotropic horizontal positional nystagmus
Conclusion
HSC-BPPV-cu is a distinct disorder of the membranous vestibular labyrinth. Not merely the lateralization but the identification of the side of the cupula to which otoconial debris is adherent has a bearing on its management. The physical therapy and maneuvers either employ the inertial forces generated by the maneuvers (e.g., HSM, mastoid oscillation, and 180-degree head-rolling maneuver) or the gravitational force (e.g., FPP) or a combination of the two for disengaging the otoconial debris adhering to the gelatinous cupula. Immediate alleviation of vertigo and disappearance of the apogeotropic horizontal PN after HSM suggests Cup-U variant of the disorder (cases 1,2, and 3) as the otoconial debris detached from the utricular side of the cupula disperses in the gelatinous matrix of the utricle. Failure to resolve the positionally triggered vertigo and nystagmus after HSM may occur when the otoconial debris is either still tightly adherent to the cupula (on any side) or else in the Cup-C variant in which disengagement transforms cupulolithiasis into canalolithiasis. A transformation from Cup-C cupulolithiasis to posterior long arm canalolithiasis (case 4) is attributed to combining different physical therapies (HSM, mastoid oscillation, 180-degree head-rolling maneuver, and FPP), and auditing its effect by an immediate SRT.
The American Academy of Otolaryngology, Head, and Neck Surgery Foundation (AAO-HNSF) clinical published guidelines for BPPV46 found insufficient evidence to recommend a preferred physical therapy for the HSC-BPPV-cu. Future randomized controlled trials are expected to address the segregation of the cases of apogeotropic HSC-BPPV due to short anterior arm canalolithiasis from those secondary to cupulolithiasis of the HSC.
Disclaimers
The views expressed in the submitted article are author's own and not an official position of the institution to which author is affiliated.
Funding
None.
Declaration of Interest
The author has no conflict of interest or disclosures to eport.
Conflict of Interest
The authors whose names are listed above certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgments
To Mr. Renith Kurian who video recorded the diagnostic and therapeutic maneuvers and precisely captured the nystagmus during the entire diagnostic and treatment period and to Mr. Ashraf Hussain for drawing ►Fig. 1 on CorelDraw graphics suite 2019.
References
- Diagnose von Krankheitserscheinungen im Bereiche des Otolithenapparatus. Acta Otolaryngol. 1921;2:434-437.
- [CrossRef] [Google Scholar]
- The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45(6):341-354.
- [CrossRef] [Google Scholar]
- Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. 1992;102(9):988-992.
- [CrossRef] [PubMed] [Google Scholar]
- Otoconia and otolithic membrane fragments within the posterior semicircular canal in benign paroxysmal positional vertigo. Laryngoscope. 2017;127(3):709-714.
- [CrossRef] [PubMed] [Google Scholar]
- Persistent direction-changing positional nystagmus: another variant of benign positional nystagmus? Neurology. 1995;45(7):1297-1301.
- [CrossRef] [PubMed] [Google Scholar]
- Horizontal canal benign paroxysmal positioning vertigo (h-BPPV): transition of canalolithiasis to cupulolithiasis. Ann Neurol. 1996;40(6):918-922.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo. In: Kountakis SE, ed. Encyclopedia of Otolaryngology, Head and Neck Surgery. Berlin, Heidelberg: Springer; 2013. p. :290-303.
- [CrossRef] [Google Scholar]
- Diagnosis and management of benign paroxysmal positional vertigo (BPPV. CMAJ. 2003;169(7):681-693.
- [Google Scholar]
- BPPV of the horizontal canal. J Neurol Neurosurg Psychiatry. 1996;60(1):68-71.
- [CrossRef] [PubMed] [Google Scholar]
- Variables affecting treatment in BPPV. Laryngoscope. 2000;110(11):1921-1924.
- [CrossRef] [PubMed] [Google Scholar]
- Occurrence of semicircular canal involvement in BPPV. Otol Neurotol. 2002;23(6):926-932.
- [CrossRef] [PubMed] [Google Scholar]
- Natural course of the remission of vertigo in patients with BPPV. Neurology. 2005;64(5):920-921.
- [CrossRef] [PubMed] [Google Scholar]
- BPPV and variants: improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005;133(1):107-112.
- [CrossRef] [PubMed] [Google Scholar]
- What is the true incidence of horizontal semicircular canal BPPV. Otolaryngol Head Neck Surg. 2006;134(3):451-454.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of BPPV in Korea: a multicenter study. J Korean Med Sci. 2006;21(3):539-543.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior canal BPPV: an underappreciated entity. Otol Neurotol. 2007;28(2):218-222.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of horizontal canal BPPV as a function of the duration of symptoms. Otol Neurotol. 2009;30(2):202-5.
- [CrossRef] [PubMed] [Google Scholar]
- Management of benign paroxysmal positional vertigo not attributed to the posterior semicircular canal: a case series. Ann Indian Acad Neurol. 2019;22(4):533-535.
- [CrossRef] [PubMed] [Google Scholar]
- Demographic and clinical characteristics of BPPV patients: a retrospective large cohort study of 1599 patients. J Otolaryngol ENT Res. 2020;12(1):20-30.
- [CrossRef] [Google Scholar]
- Benign paroxysmal positional vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vestib Res. 1996;6(3):173-184.
- [Google Scholar]
- About nystagmus transformation in a case of apogeotropic lateral semicircular canal benign paroxysmal positional vertigo. Int J Otolaryngol. 2011;2011:687921.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of benign paroxysmal positional vertigo. A clinical review. J Otol. 2017;12(4):165-173.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo of the horizontal canal. Clin of Otorhinolaryngology. 2017;1(1):7-14.
- [Google Scholar]
- Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. 2005;25(5):277-283.
- [Google Scholar]
- Positional vertigo and ageotropic bidirectional nystagmus. Laryngoscope. 1997;107(6):807-813.
- [CrossRef] [PubMed] [Google Scholar]
- Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3-4):105-117.
- [CrossRef] [PubMed] [Google Scholar]
- A single therapy for all subtypes of horizontal canal positional vertigo. Laryngoscope. 2005;115(8):1432-1435.
- [CrossRef] [PubMed] [Google Scholar]
- Bedside therapeutic experiences with horizontal canal benign paroxysmal positional vertigo (cupulolithiasis. Acta Otolaryngol. 2009;129(11):1217-1221.
- [CrossRef] [PubMed] [Google Scholar]
- A cupulolith repositioning maneuver in the treatment of horizontal canal cupulolithiasis. Auris Nasus Larynx. 2012;39(2):163-168.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized clinical trial for apo- geotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;78(3):159-166.
- [Google Scholar]
- New treatment strategy for cupulolithiasis associated with benign paroxysmal positional vertigo of the lateral canal: the head-tilt hopping exercise. Eur Arch Otorhinolaryngol. 2014;271(12):3155-3160.
- [CrossRef] [PubMed] [Google Scholar]
- New treatment strategy for apogeotropic horizontal canal benign paroxysmal positional vertigo. Audiology Res. 2016;6(2):163.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of mastoid oscillation and the Gufoni maneuver for treating apogeotropic horizontal benign positional vertigo: a randomized controlled study. J Neurol. 2017;264(5):848-855.
- [CrossRef] [PubMed] [Google Scholar]
- Physiologische Untersuchungen Ueber das Endorgan de Nervus Octavus. Wiesbaden, Germany: Bergmann JF Publishers; 1892.
- [Google Scholar]
- Converting apogeotropic into geotropic lateral canalolithiasis by head-pitching manoeuvre in the sitting position. Acta Otorhinolaryngol Ital. 2008;28(6):287-291.
- [Google Scholar]
- Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol Neurotol. 2005;26(2):257-260.
- [CrossRef] [PubMed] [Google Scholar]
- “Secondary signs of lateralization” in apogeotropic lateral canalolithiasis. Acta Otorhinolaryngol Ital. 2010;30(2):78-86.
- [Google Scholar]
- The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112(1):172-178.
- [Google Scholar]
- The physical treatment of lateral semicircular canal canalolithiasis. Audiol Med. 2005;3(1):52-56.
- [CrossRef] [Google Scholar]
- The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 1998;118(4):455-460.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practice guideline: benign paroxysmal positional vertigo. (update. Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1-S47.
- [Google Scholar]







