Translate this page into:
The Effect of Epidermal Growth Factor on the Outcomes of Myringoplasty
Address for correspondence Vikram Kemmannu Bhat, MS, DNB, MNAMS, PhD, Department of Otolaryngology, Head and Neck Surgery, Karnataka Institute of Medical Sciences, Vidyanagar, Hubli 580021, Karnataka, India (e-mail: vikram.ent@gmail.com).
Abstract
Introduction
Chronic otitis media is a widespread disease of developing countries. The burden of the disease continues to be high and so is the demand for surgical myringoplasty. This pilot study aimed to compare in adults the outcomes of myringoplasty with and without the application of epidermal growth factor gel (EGF) with respect to the time taken for graft uptake, improvement of hearing, and complications.
Materials and Methods
This randomized controlled study was undertaken in a tertiary referral public hospital in a span of 2 years with a sample size of 60 patients. All of them underwent diagnostic nasal endoscopy, otoendoscopy, and pure tone audiometry and treated with conventional underlay myringoplasty using temporalis fascia (Group A—30 cases with EGF, Group B—30 controls without EGF). Patients were followed-up at 15, 30, 90 days postoperatively.
Results
The average time taken for closure of tympanic perforation and graft uptake by group A was lesser than group B. This difference was found to be statistically significant. Residual perforation at 1 month was commoner in group B as compared with group A. The final improvement of the hearing was the same in both the groups in the healed cases.
Conclusion
The EGF can be used to improve the outcomes of myringoplasty. It can hasten the closure of tympanic membrane perforation and increase the success rates of the surgery.
Keywords
chronic otitis media
myringoplasty
epidermal growth factor
hearing loss
Introduction
Chronic otitis media (COM) is a widespread disease of developing countries. The burden of the disease continues to be high and so is the demand for surgical myringoplasty. However, surgical myringoplasty takes its own time to perform and hence it is difficult to post many cases in a day. There is already some evidence from our previous study of epidermal growth factor (EGF) gel being useful in the healing of tympanic membrane perforation.1 Hence in this study, we tried to find out if EGF could promote the healing process and shorten the recovery period in tympanoplasty. This pilot study aimed to compare the outcomes of myringoplasty with and without the application of EGF with respect to the time taken for graft uptake, improvement of hearing, and complications in adults.
Materials and Methods
This randomized controlled pilot study was undertaken in a tertiary referral teaching hospital after clearance from the Institutional Review Board (PGS/KIMS/139/2016–17) in a span of 2 years with a sample size of 60. The patients were divided into 2 groups—Group A:30 cases with EGF, Group B: 30 controls without EGF. The inclusion criteria included perforations in the pars tensa due to mucosal COM or trauma in adults. Patients with active mucosal COM or a predisposing disease focus on nose or throat were excluded from the study. Tuberculous, diabetic, or immunocompromised patients were excluded too. Every consecutive eligible patient was recruited into the study. Ralloc software was used to randomize the patients and allocation concealment was also incorporated to reduce bias. All patients underwent diagnostic nasal endoscopy, Eustachian tube function tests, otoendoscopy, and pure tone audiometry (PTA) before surgery.
Patients in both groups underwent conventional underlay myringoplasty by postaural approach with autologous temporalis fascia. The decision to apply EGF after placement of the graft was confirmed only after the concealed envelope was opened. Small paper slips containing the codes 1 or 2 would be displayed to the surgeon. Number 1 was for EGF while, 2 for without EGF. All surgical procedures were performed by two experienced surgeons with similar skills. One gram of EGF (Regen-D® 150 μg/g manufactured by Bharat Biotech International Ltd, Hyderabad, India) was mixed with small pieces of gel foam (Absorbable gelatin sponge; Virchow Biotech Private Ltd., Ranga Reddy District, Andhra Pradesh, India) and delicately arranged in a peripheral circle over the temporalis fascia. The external ear canal was then packed with Povidone Iodine tulle (Povi-10™ containing Povidone Iodine IP 10% w/w, Ornidazole IP 1% w/w manufactured by Nemus Pharmaceuticals Pvt Ltd, India). Mastoid dressing was done finally. All patients were treated with antibiotic injections according to the preoperative ear swab culture report. They were discharged on the seventh day after the removal of sutures.
Patients were followed up after 15, 30, and 90 days in the outpatient clinic by a neutral observer and the outcomes recorded. PTA was done at 30 and 90 days. Duration for the reduction in size or closure of perforation was the primary outcome. The size of the perforation was recorded before and after (If any) surgery endoscopically at a fixed distance from the tympanic membrane. The images were analyzed using “Image j" software. A ratio of the area of the perforation to the area of the tympanic membrane was obtained as a percentage. Improvement in hearing (PTA), development of aftereffects like tympanosclerosis, atrophy, or pus formation during follow-up were the secondary outcomes considered.
Intention to treat analysis was employed and CONSORT statement guidelines were followed in reporting the study (► Fig. 1). The data were tabulated into tables and analyzed using a chi-square test. The level of significance was set at 95% confidence intervals.
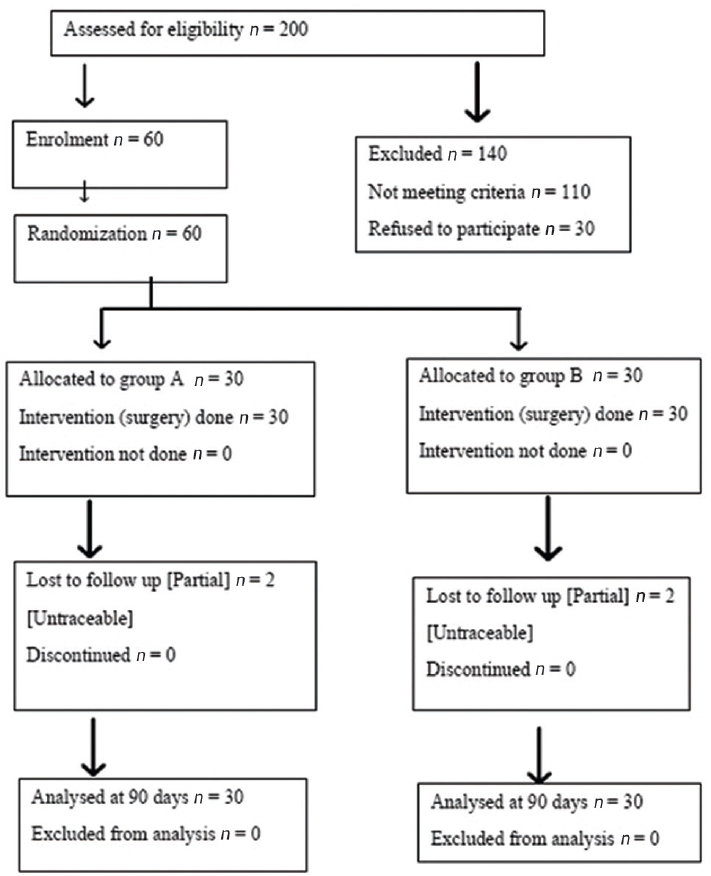
- CONSORT flowchart showing study details.
Results
The mean age of cases and controls was 26.1(10.6) years and 27.0 (11.0) years respectively and there was no statistically significant difference in age. Of the total 30 cases, 19 were female (63.3%) and among controls, 18 were female (60%) and this difference was not significant (p-value 0.789). The average time taken for closure of tympanic perforation and graft uptake by group 1 was lesser than group 2. This difference was found to be highly significant (► Table 1). Residual perforation at 30 and 90 days was commoner in group 2 as compared with group 1. The final improvement of the hearing was the same in both the groups in the healed cases (► Table 2). The graft uptake and perforation closure rates at the end of 30 days were 70 and 30% in group 1 and group 2, respectively. The same at the end of 90 days was 93.33 and 73.33%. However, this was not found to be statistically significant (► Table 3). The quality of healing was better in group A as compared with group B. This difference was again statistically insignificant (► Table 4). No complications related to the application of EGF were noticed in this study.
| Approximate duration for the healing of tympanic perforation | Group A n | Group B n | Total |
|---|---|---|---|
| 15 d | 8 | 0 | 8 |
| 15–30 d | 13 | 9 | 22 |
| 31–90 d | 7 | 13 | 20 |
| >90 d | 2 | 8 | 10 |
| Total | 30 | 30 | 60 |
Note: Chi-square test p = 0.004.
| Hearing improvement | Group A n | Group B n | Total |
|---|---|---|---|
| 30 d | 8 | 4 | 12 |
| 90 d | 8 | 11 | 19 |
| >90 d | 14 | 15 | 29 |
| Total | 30 | 30 | 60 |
Note: Chi-square test p = 0.389.
| Healing of perforation after 1 month | Group A n | Group B n | Total |
|---|---|---|---|
| Complete | 17 | 8 | 25 |
| Partial | 11 | 17 | 28 |
| No difference | 2 | 5 | 7 |
| Total | 30 | 30 | 60 |
Note: Chi-square test p = 0.054.
| Quality of healing of perforation after 1 month | Group A n | Group B n | Total |
|---|---|---|---|
| Good | 13 | 4 | 17 |
| Fair | 9 | 9 | 18 |
| Poor | 1 | 4 | 5 |
| Total | 23 | 17 | 40 |
Note: Chi-square test p = 0.055.
Discussion
COM is one of the commonest causes of hearing loss that results mainly due to tympanic membrane perforation. The burden of tympanic perforation due to infection or trauma continues to be high in the developing countries despite the improvement in the standard of living. Many patients are reluctant to undergo surgical procedures for a painless perforation because of the long hospital stay and morbidity involved in the corrective procedures. This often leads to procrastination of treatment and neglect of ear disease for many years. The use of EGF helps to reduce the healing time for tympanic perforation after myringoplasty and hence reduces the duration of hospital stay. A comparison is made with recent other studies on humans using EGF and platelet-rich plasma (PRP) in ► Table 5. Our results are in agreement with that of Lou et al2 who found reduced healing time in traumatic perforations. A study previously performed by us had proved the efficacy of EGF in nonhealing tympanic membrane perforations.1 Zhengcai-Lou et al3 suggested the use of a combination of EGF and basic fibroblast growth factor for the formation of epithelium and fibrous layer during tympanic membrane regeneration. Djamin et al4 used amniotic membrane as graft and EGF on chronic perforation of TM.
| Sl. no | Year | Author | Study design | n | Results |
|---|---|---|---|---|---|
| 1 | 2019 | Lou8 | Case series | 26 | 100% closure rate after 6 month |
| 2 | 2018 | Bhat et al1 | Randomized control trial | 80 | 71.42% success rate in group with EGF and silver nitrate and 47.36% in group with only silver nitrate |
| 3 | 2018 | Lou et al2 | Cohort study Retrospective | 95 | 92.6% closure rate at 6 month with daily topical EGF application |
| 4 | 2018 | Djamin et al4 | Randomized control study | 20 | Faster decrease in perforation diameter in group with EGF than in group without EGF |
| 5 | 2016 | Yang et al9 | Retrospective | 120 | 93.5% closure rate in group with EGF, 92% in group with ofloxacin otic drops and 82.2% in observation group |
| 6 | 2016 | Lou et al10 | Randomized control study | 97 | Closure time 25.1 ± 10.5 d in group without EGF and 11.7 ± 5.2 d in group with EGF |
| 7 | 2016 | Lou et al3 | Randomized study | 86 | 86.2% closure rate in group with EGF and 72.4% in observation group |
| 8 | 2020 | Taneja et al11 | Randomized control study | 22 | 95.1% healing in PRP group and 85.3% in control group after 6 month |
| 9 | 2020 | Ersozlu and Gultekin7 | Case–control study | 63 | 100% success rate in group with PRP and 83.8% in control group |
| 10 | 2018 | Sharma et al12 | Randomized observational study | 100 | 92% healing in PRP group and 64% in control group after 3 month |
| 11 | 2016 | Gür et al13 | Randomized study | 60 | 93% healing in PRP group and 83% in paper patching group |
| 12 | 2015 | El-Anwar et al14 | Randomized control trial | 64 | 100% graft taking in cases and 81.25% in control group |
Abbreviations: EGF, epidermal growth factor; PRP, platelet-rich plasma.
They found that EGF had a role in shrinking the perforation diameter. We too have observed the same and noticed that EGF helped reduce the size of the perforation, if not closing it completely.
The effective dose of EGF and the number of applications for the closure of perforation needs to be titrated and studied further. Ramsay et al5 tried EGF (0.25 mg/mL) on chronic perforations and found that higher concentrations with the stripping of perforation edges were required to improve healing. A mechanism for the sustained release of EGF eliminates the need for repeated applications. Seonwoo et al6 used a chi- tosan patch for sustained release of EGF. They found this to be much better than spontaneous healing in TM perforations of humans.
Higher surgical success rates have been reported by all of them in ► Table 5 who used PRP. Ersozlu and Gultekin et al7 claimed 100% success rates with PRP gel fat graft myringoplasty in 4 months follow-up. However, there was no difference in audiological results. Preparation of PRP is a laborious time-consuming process that requires the support of a blood bank or a laboratory with a centrifuge. EGF has the advantage of being a readymade preparation and does not need to be separately prepared for every individual patient. However, EGF has the disadvantage of being heat-labile and also expensive.
Conclusion
The EGF can be used to improve the outcomes of myringoplasty. It can promote and hasten the closure of tympanic membrane perforation and increase the success rates of the surgery.
Conflict of Interest
None declared.
References
- Effect of silver nitrate and epidermal growth factor on nonhealing tympanic membrane perforations: a randomized controlled study. Ann Otol Neurotol. 2018;1:29-33.
- [CrossRef] [Google Scholar]
- Pretreatment factors affecting traumatic tympanic membrane regeneration therapy using epidermal growth factor. Am J Otolaryngol. 2018;39(6):711-718.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study on the effects of EGF and bFGF on the healing of human large traumatic perforations of the tympanic membrane. Laryngoscope. 2016;126(1):E23-E28.
- [CrossRef] [Google Scholar]
- Topical application of epidermal growth factor (EGF) to changes in tympanic membrane perforation diameter. J Med Sci. 2018;18:186-191.
- [CrossRef] [Google Scholar]
- Effect of epidermal growth factor on tympanic membranes with chronic perforations: a clinical trial. Otolaryngol Head Neck Surg. 1995;113(4):375-379.
- [CrossRef] [PubMed] [Google Scholar]
- Regeneration of chronic tympanic membrane perforation using an EGF-releasing chitosan patch. Tissue Eng Part A. 2013;19(17-18):2097-2107.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of the autologous platelet rich plasma gel fat myringoplasty and the fat graft myringoplasty for the closure of different sizes of tympanic membrane perforations. ENT J. 2020;99(5):331-336.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of epidermal growth factor on the pseudohealing of traumatic tympanic membrane perforations. Rev Bras Otorrinolaringol (Engl Ed) 2019 Doi: 10.1016/j.bjorl.2019.06.011
- [Google Scholar]
- A retrospective study of EGF and ofloxacin drops in the healing of human large traumatic eardrum perforation. Am J Otolaryngol. 2016;37(4):294-298.
- [CrossRef] [PubMed] [Google Scholar]
- Topical application of epidermal growth factor with no scaffold material on the healing of human traumatic tympanic membrane perforations. Clin Otolaryngol. 2016;41(6):744-749.
- [CrossRef] [PubMed] [Google Scholar]
- Role of platelet rich plasma in tympanoplasty. Indian J Otolaryngol Head Neck Surg. 2020;72(2):247-250.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of platelet rich fibrin in myringoplasty. Int J Otorhinolaryngol Head Neck Surg. 2018;4:677-681.
- [CrossRef] [Google Scholar]
- Use of a platelet-rich fibrin membrane to repair traumatic tympanic membrane perforations: a comparative study. Acta Otolaryngol. 2016;136(10):1017-1023.
- [CrossRef] [PubMed] [Google Scholar]
- Topical use of autologous platelet rich plasma in myringoplasty. Auris Nasus Larynx. 2015;42(5):365-368.
- [CrossRef] [PubMed] [Google Scholar]







